Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124


Source: Kaboompics/Pexels
Supporting clients who are at risk of suicide is one of the most important things we do. stressful Difficult aspects of clinical practice. The responsibility to ensure client safety, while recognizing that client behavior is ultimately beyond control, can be overwhelming for even the most experienced clinician. This series on suicide assessment focuses on conceptual and practical assessment approaches designed to help clinicians respond effectively when clients share thoughts of suicide. Focus on assessing and building “immediate safety” confidence It’s about having a clear plan to maintain that safety. This series consists of three parts.
Although there is no single cause of suicide, certain factors are known to increase the risk of an attempt, and understanding these factors is essential for effective suicide care. Simply put…
What’s important to note when considering risk factors and warning signs is the sheer number of points that need to be considered in the assessment process. For clinicians, the following questions arise:
What should I do about this? Almost anything a person experiences can put them at risk for suicide.
One helpful way to look at all of these risk factors and the assessment itself is through the lens of the 988 Suicide and Crisis Lifeline Safety Assessment Model.2. This model includes what are called the four core principles of suicide assessment (see Joiner et al., 2007), which help group these risk factors into a more useful and easy-to-use framework. Masu. These principles are based on the Interpersonal Psychological Theory of Suicide (IPTS) (Joiner 2005), which proposes that: suicidal Purposeful desires and acquired abilities are associated with increased risk of suicide.
Joyner’s theory is that feeling like a burden or experiencing social alienation can create a desire to die, and that once an individual makes plans or begins preparatory actions, the desire to die can We propose that this desire may progress. However, Joyner argues that in order to act on this desire, we need to overcome our innate desire. fear of death–He calls this process “acquiring the capacity” to die. This ability develops through repeated exposure to painful or provocative experiences, including past suicide and non-suicidal attempts. self-harm, traumaor physical pain. Joyner’s groundbreaking research explains how suicidal thoughts arise and why many people with such thoughts do not attempt suicide, or have not acquired the ability to commit suicide. There is.
The four guiding principles focus on these areas (desire, intent, and ability), with buffers added to consider factors that may help reduce that risk. The table below shows how risk factors/warning signs are grouped based on these basic principles.3
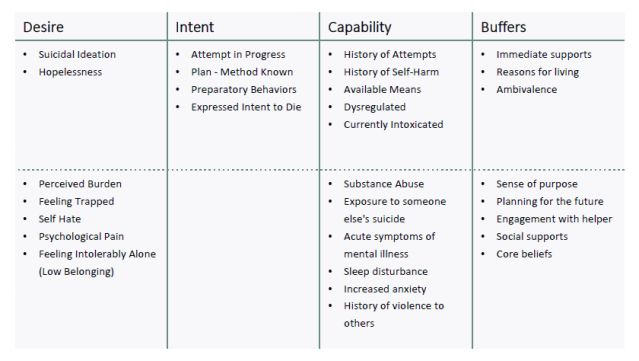
Four core principles of suicide assessment
Source: 988 Suicide and Crisis Lifeline Safety Assessment
When evaluating based on these four fundamental principles, we focus on:
How does grouping elements like this help your evaluation?
When assessing suicide risk in clinical practice, this framework directs: Note Four key elements:
What do you know about your client’s desires, intentions, capabilities, and buffers?
This is what I find most convenient. In a potentially stressful moment, when a client is sharing thoughts about suicide, instead of recalling all possible risk factors or following a lengthy screening tool, I focus on: Masu. Desire, intention, ability, buffer.
When a client expresses suicidal thoughts (desires), I immediately consider their thoughts. intention and ability. To better understand the strength of these ideas, I often ask them to rate them. desire For example, a rating of 7 or 8 indicates a strong desire to die.
The next thing to think about is intention To act. A similar rating of 7 or 8 alerts you to increased risk. A low rating can provide some reassurance that suicidal thoughts are present, but the intention to act is not strong.
Regardless of my assessment of desire or intent, when a client is thinking about suicide, I always assess as follows: ability. This includes considering any history of self-harm or self-harm, and discussing access to resources. Both are essential to understanding risks and determining appropriate responses.
Asking clients to rate the intensity of their experiences is not a standard part of this framework, but can be a valuable tool for self-reflection. This allows the client to pause and consider the seriousness of the suicidal ideation, while providing the clinician with additional insight into intent. The evaluation itself does not determine a course of action. Instead, they guide the conversation and create opportunities to demonstrate that open discussion about suicidal thoughts is safe and encouraged. The reality is that many people experience suicidal thoughts without the intention to act or the precautions of hearing aids.
In our next post, we’ll discuss how to start collecting the information you need for a complete evaluation, focusing on the following methods: listen About suicide listen Use the framework you outlined to match your client’s story. reveal Are there any gaps in assessment data?